God’s Design: Strategic Routing of the RLN
The recurrent laryngeal nerve’s detour serves an important designed function
Abstract
Evolutionists often cite the recurrent laryngeal nerve (RLN) as evidence of “poor design.” This article evaluates the physiological role of the RLN in its innervation and regulation of the larynx (voice box). Beyond the larynx’s role in speech, it plays a vital role in regulating the flow of air into the trachea (windpipe) and food into the esophagus (food pipe). A closer look at the RLN reveals that, in its “detour” around the subclavian artery on the right and the aortic arch on the left, there are many additional branches that interact with not only the heart and aorta but cervical regions of the trachea and esophagus—organs that depend intimately on the functionality of the larynx to protect the airway and promote swallowing. The rare incidences of non-recurrence in the RLN, as well as incidences of damage to the RLN, afford a means to explore the critical role these afferent pathways play in the coordination of these functions. Embryological developmental constraints are considered as well—particularly, the role the recurrent nature of the RLN may play in the closure of the ductus arteriosus after birth. This supporting evidence makes it difficult to believe that the placement of the RLN was a mistake or a coincidence but rather a detour by design. The scientific community is encouraged to delve deeper into the role of afferent innervations of the RLN in support of healthy physiological functions.
Main Points
- Anatomy: The role of peripheral nerves and the anatomy of the RLN is reviewed.
- Evolutionary Claim: Evolutionists cite the recurrent nature of the RLN as evidence of “poor design.”
- Role of the Larynx: The vital role of the larynx is addressed, which is innervated by the RLN.
- Evidence of Design: Evidence supports the value of the recurrent nature of the RLN, which innervates the aorta, heart, trachea and esophagus, as well, upon its return route.
- Critical Afferent Inputs: Afferent sensory information is transmitted to the brain that is critical to the functionality of the larynx—regulating breathing and eating.
- Developmental Constraints: Embryological developmental constraints may play a role in the anatomical placement of the RLN, but that does not infer “poor design” or lack of a designer.
- Embryological Significance: The unique position of the RLN may play a critical role in the closure of the ductus arteriosus after birth.
- Impact on Scientific Discovery: Evolutionary ideology hinders scientific discovery; evaluation of the role of afferent inputs from the RLN may provide further evidence of design.
Did you ever play telephone as a kid using two tin cans with a string between them? Okay, so I may be showing my age, but in my day, it was great fun to whisper secret conversations from tree fort to tree fort via this not-so-sophisticated form of communication. Messages could be sent back and forth, and the sound was carried through the fibers of the string. While far more sophisticated, the nervous system works in much the same way. Peripheral nerves are made of bundled axons that connect nerve cell bodies in the brain with distant tissues and organs. Commands and sensory information are conveyed to and from the extremities in this way.
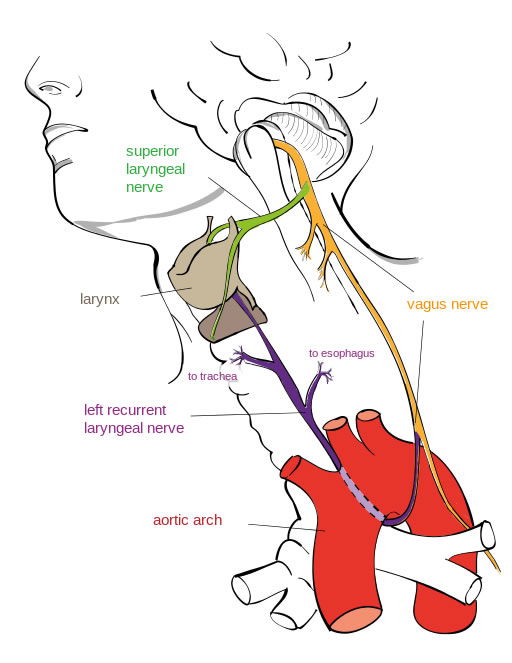
Figure 1. Anatomy of the recurrent laryngeal nerve. The RLN is strategically positioned in amongst the esophagus and trachea. Illustration by Jkwchui (Based on drawing by Truth-seeker2004), via Wikimedia Commons.
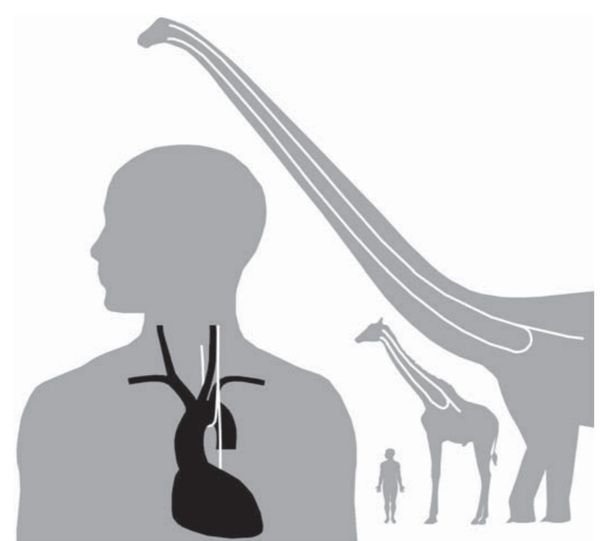
Figure 2. RLN comparisons.2
Isn’t This the Long Way?
While most nerves have a more-or-less direct route to their end organ, the recurrent laryngeal nerve (RLN) is a branch of the vagus nerve that seems to get sidetracked en route to the larynx (voice box). Evolutionists have long cited this as a primary example of “poor design.”1
The RLN takes what would appear to be an unnecessary loop around the right subclavian artery on the right side and the aortic arch on the left before returning up to the tracheoesophageal groove and then the larynx (Figure 1). Both are much longer than they would “need” to be—the left being seven times longer than if it traveled a direct course from the head to the neck. This is exaggerated in animals with long necks. In the giraffe, the RLN can be more than 15 feet long—just imagine a brachiosaurus (Figure 2)! So, why would God do such shoddy work? Surely there is no designer, the evolutionists declare. But wait . . . .
Gathering Intel
Maybe a direct route isn’t always the best route. Remember, the nerves not only carry commands from the brain to the end organ, but they also carry sensory and visceral inputs to the brain to elicit an appropriate response. Imagine an army commander who only gave orders without receiving any input from the troops out in the trenches. Now that would surely be a disaster. In the nervous system, afferent neurons carry information from “the trenches” to the brain so that appropriate responses can be signaled back out to the field via efferent neurons. Loss of this essential chain of information can have significant implications.
In the case of the RLN, communication is between the brain and the larynx. The larynx, often referred to as the voice box, is a unique and vital organ that is not only involved with speech production but also regulates the flow of air into the trachea (windpipe) as well as liquids and food into the esophagus (food pipe). That is an important job, to be sure. If you have ever had something go down the “wrong pipe”—that disconcerting moment where food or water is inadvertently sent down the windpipe, leaving you gasping and sputtering—you quickly realize just how important a job it is. While we can make a recovery from such an event, clearly, we would not want this to happen often. Indeed, it could prove fatal. We take for granted how seamlessly this usually happens . . . all because of the good information from “the field.” Anatomical and clinical research suggests that information gathered by the RLN on its “superfluous detour” is actually essential to the regulation of this most vital function of the larynx.
Anatomically, it is evident that the RLN supplies numerous autonomic and sensory nerves as it travels back up toward the larynx, branching off to the aorta, heart, esophagus, and trachea.3 The positioning of the RLN, looped around the aortic arch and the subclavian artery, nestles it right amongst the very organs it needs to gather information from (Figure 2). Beyond its innervation of the vocal folds for speech, there are sensory, secretory, and motor fibers to segments of the esophagus and the trachea that lie beyond the larynx itself.4 Indeed, it returns to the larynx via the tracheoesophageal groove—clearly showing its intimate association with these organs. This should not be surprising considering the critical job of the larynx as it coordinates the activities of these two organ systems—allowing us to eat and breathe . . . just not at the same time!
Failure to Report
One interesting way to assess the importance of the recurrence of the RLN is to observe when it isn’t recurrent. There are some rare cases where there is non-recurrence in the RLN (NRLN), particularly in the right RLN. An aberration of the subclavian artery during embryological development creates a situation where the RLN is no longer drawn down into the chest cavity with the developing heart and lungs. Rather, there is a more direct innervation of the larynx—avoiding the “detour.” This only happens in about 0.3–0.8% of individuals.
It is even more rare to have a non-recurrent laryngeal nerve on the left side (0.004%). Indeed, it has only been observed in the case of situs inversus, which is the reversal of the internal organs—heart on the right, appendix on the left, etc. So, essentially, a left non-recurrent laryngeal nerve is just a right non-recurrent laryngeal nerve—that happens to end up on the left side. This anomaly is observed with an aberrant subclavian artery once again. In both cases, the opposite RLN is still recurrent and looped under the aortic arch.
Individuals with NRLNs have been reported to exhibit difficulty swallowing and foreign body sensation during swallowing
Returning to the analogy of the army commander receiving information from the field, in this case, the commander (the brain) is getting limited information from “the field.” Perhaps it is not surprising, then, to find that individuals with NRLNs have been reported to exhibit difficulty swallowing and foreign body sensation during swallowing5—suggesting a role for the recurrent path of this nerve in the optimal functioning and regulation of the larynx and the associated organs beyond, such as the esophagus.
Instances where the RLN has been injured offer additional support for the purpose or usefulness of recurrence in this particular nerve. Numerous studies have investigated damage to the RLN, often due to surgical complications, tumors, or endotracheal intubations.6 As would be expected, bodily functions associated with the larynx are affected, including an impaired ability to protect the airway leading to aspiration, pneumonia in some cases, dysphagia, or difficulties in clearing the throat and swallowing.7
While these may be explained by a lack of communication directly to the larynx, studies also suggest that the loss of afferent information from the organs it encounters on its “detour” also plays an important role. For example, one study found that initiation of the esophageal phase of swallowing (beyond the larynx) is determined by feedback from peripheral reflexes, which are mainly conveyed via afferents from the esophagus through the RLN.8 Others have found that connections between the afferent sensory fibers of the RLN, the motor neurons of the RLN, and the motor nuclei of the hypoglossal nerve are vital to the integrity of safe swallow function.9
Stagnant or Strategic?
Evolutionists,10 as well as some creationists,11 often cite constraints imposed during embryological development as the reason for the conservation of the recurrence of the RLN. The evolutionist might claim that “the only reasonable explanation for the route of the nerve is that it originally started out innervating gills in fish.”12 On the other hand, a creationist might say it is “the necessary consequences of developmental dynamics”13—the need to remain functional throughout development—not historical carryovers from evolution.
Observing the various stages of embryological development may suggest the positioning of the RLN could be related to this process. However, even if this should play a role, it does not necessarily infer “poor design” or lack of a designer. If you have watched HGTV at all, you have likely seen a show where they are designing the layout of a house. There are times when a design feature precludes what may be the most direct route for something else. For example, installing a brick fireplace in a family room may preclude the most desirable placement of electrical circuitry, but that does not mean that the designer was not intelligent. Sometimes, a designer needs to make choices regarding what is the most important or desired feature—which may come at the expense of other, practical decisions.
Sometimes, a designer needs to make choices regarding what is the most important or desired feature—which may come at the expense of other, practical decisions.
In support of this concept, the closure of the ductus arteriosus at the time of birth could provide evidence of the strategic placement of the RLN in embryological development. A baby, for obvious reasons, cannot breathe air in the womb. Therefore, it gets its oxygen directly from the mother through the placenta. The ductus arteriosus is a fetal artery that connects the aorta and the pulmonary artery. It carries oxygenated blood directly to the baby’s body, bypassing the lungs for the time being. However, when a newborn breathes and begins to use its lungs at birth, the ductus is no longer needed and usually closes by itself during the first two days after birth. If this does not occur, the result is a mixing of oxygen-rich blood and oxygen-poor blood, which strains the heart and pulmonary arteries. So, this begs the question: How does this artery close?
A study that is nearly 40 years old examined the walls of the aortic arch in embryos and fetuses at varying stages of development.14 It was observed that the structure of the wall of the aortic arch was different in the region where the vagus and the RLN supported it and that this allowed it to develop as a more muscular, rather than elastic, vessel that likely contributed to the closure of the ductus arteriosus. So, while related to so-called embryological constraints, the unique positioning of this odd, recurrent nerve may not be so poorly designed.
Detour in Discovery
This entire discussion begs that some critical questions be considered—if not answered. Does the recurrence of the RLN reflect a compromise due to embryological developmental constraints or a strategical placement? Are the right and left RLNs drug down into the thorax as an evolutionary afterthought or intentionally placed there to gather and disseminate vital information from regions that critically impact the end organ—the larynx? Are the subclavian artery and the aortic arch obstacles to a more desirable design strategy or simply tools—like a crochet hook—that pull the RLN into the precise location needed to provide the best field input to the army commander? The supporting evidence makes it difficult to believe that the placement of the RLN was a mistake . . . or a coincidence.
It is troubling to consider how evolutionary indoctrination has hindered the progress of science. For years, scientists essentially ignored vast regions of DNA, declaring them “junk,” and dismissed entire organs—declaring them “vestigial.” In many cases, we are just now beginning to understand the critical role these play in the overall functioning of the human body. Well, as it turns out, God doesn’t make “junk”!
It will be interesting to learn more about how the afferent information gathered by the RLN on its “detour” affects physiological functions. This serves as a challenge to the scientific community to take its evolutionary blinders off and scientifically investigate a part of the human anatomy that has long been deemed, simply, “poor design.” They just might be surprised at what they find. The recurrence of the RLN appears to be a detour by design . . . mapped out by the Designer himself!
For you formed my inward parts;
you knitted me together in my mother’s womb.
I praise you, for I am fearfully and wonderfully made.
Wonderful are your works;
my soul knows it very well.
My frame was not hidden from you
when I was being made in secret,
intricately woven in the depths of the earth. (Psalm 139:13–15)
Answers in Depth
2022 Volume 17
Answers in Depth explores the biblical worldview in addressing modern scientific research, history, current events, popular media, theology, and much more.
Browse VolumeFootnotes
- Jerry A. Coyne, Why Evolution is True, (New York: Viking, 2009), 82–84; and Donald R. Prothero, Evolution: What the Fossils Say and Why It Matters, (New York: Columbia University Press, 2007), 37–38.
- Mathew J. Wedel, “A Monument of Inefficiency: The Presumed Course of the Recurrent Laryngeal Nerve in Sauropod Dinosaurs,” Acta Palaeontologica Polonica 57, no. 2 (May 2011): 251–256.
- Paul Rea, “Vagus Nerve,” Essential Clinical Anatomy of the Nervous System (Massachusetts: Academic Press, 2015), 10.7.1.
- Michael Schuenke, Erik Schulte, Udo Schumacher, Thieme Atlas of Anatomy: Head and Neuroanatomy (Thieme, 2007), 142–144.
- Yong Tae Hong and Ki Hwan Hong, “The Relationship Between the Non-recurrent Laryngeal Nerve and the Inferior Thyroid Artery,” Indian Journal of Surgery 80, no. 2 (April 2018): 109–112.
- David Myssiorek, “Recurrent Laryngeal Nerve Paralysis: Anatomy and Etiology,” Otolaryngologic Clinics of North America 37, no. 1 (February 2004): 25–44.
- Jennifer M. Pusins, Randi Melton, and Lily Darmon, “Recurrent Laryngeal Nerve Damage—Clinical Implications Following Cardiac Surgery,” Today’s Geriatric Medicine 12, no. 3 (May/June 2019): 20.
- Ivan M. Lang, Bidyut K. Medda, Arash Babaei, and Reza Shaker, “Role of Peripheral Reflexes in the Initiation of the Esophageal Phase of Swallowing,” American Journal of Physiology-Gastrointestinal and Liver Physiology 306, no. 8 (April 2014): G728–G737.
- Francois David Henry Gould, Jocelyn Ohlemacher, Andrew R Lammers, et al., “Central Nervous System Integration of Sensorimotor Signals in Oral and Pharyngeal Structures: Oropharyngeal Kinematics Response to Recurrent Laryngeal Nerve Lesion,” Journal of Applied Physiology 120, no. 5 (December 2015): 495–502.
- Wedel, “A Monument of Inefficiency.”
- Jerry Bergman, “Recurrent Laryngeal Nerve Is Not Evidence of Poor Design,” Acts & Facts 39, no. 8 (August 2010): 12–14.
- Jerry A. Coyne, Why Evolution is True (New York: Viking, 2009), 82–84.
- Erich Blechschmidt, The Ontogenetic Basis of Human Anatomy: A Biodynamic Approach to Development from Conception to Birth, trans. B. Freeman (New York: North Atlantic Books, 2004), 188.
- M.E. Leonard, G. M. Hutchins, and G. W. Moore, “Role of the Vagus Nerve and Its Recurrent Laryngeal Branch in the Development of the Human Ductus Arteriosus,” American Journal of Anatomy 167, no. 3 (July 1983): 313–327.
Recommended Resources

Answers in Genesis is an apologetics ministry, dedicated to helping Christians defend their faith and proclaim the good news of Jesus Christ.
- Customer Service 800.778.3390
- Available Monday–Friday | 9 AM–5 PM ET
- © 2026 Answers in Genesis